What Is Heel Discomfort And Methods To Remedy It
Overview
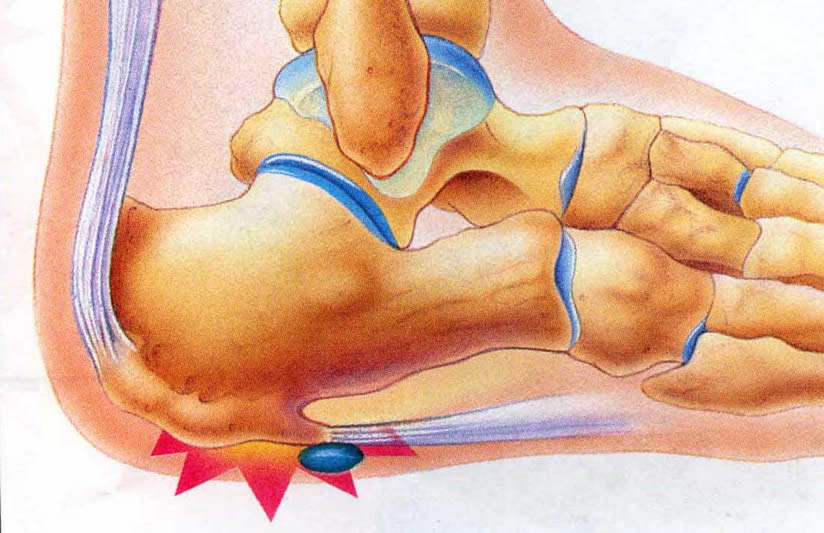
The plantar fascia is a thick, ligamentous connective tissue that runs from the heel bone to the ball of the foot. This strong and tight tissue helps maintain the arch of the foot. It is also one of the major transmitters of weight across the foot as you walk or run. Thus, tremendous stress is placed on the plantar fascia, often leading to plantar fasciitis- a stabbing or burning pain in the heel or arch of the foot. Plantar fasciitis is particularly common in runners. People who are overweight, women who are pregnant and those who wear shoes with inadequate support are also at a higher risk. Prolonged plantar fasciitis frequently leads to heel spurs, a hook of bone that can form on the heel bone. The heel spur itself is not thought to be the primary cause of pain, rather inflammation and irritation of the plantar fascia is the primary problem.
Causes
It usually starts following an increase in activity levels. Increase in weight. Standing for long periods. Poor footwear. Tight muscle groups. Abnormal pressure on the plantar Fascia can be caused by any of the above. The plantar fascia becomes inflamed and tiny rips can occur where it attaches into the inside of the heel bone. The area becomes inflamed and swollen, and it is the increase in fluid to the area that accumulates when weight is taken off the area that then causes the pain on standing.
Symptoms
You'll typically first notice early plantar fasciitis pain under your heel or in your foot arch in the morning or after resting. Your heel pain will be worse with the first steps and improves with activity as it warms up. As plantar fasciitis deteriorates, the pain will be present more often. You can determine what stage your are in using the following guidelines. No Heel Pain, Normal! Heel pain after exercise. Heel pain before and after exercise. Heel pain before, during and after exercise. Heel pain all the time. Including at rest! This symptom progression is consistent with the four stages of a typical overuse injury. Ultimately, further trauma and delayed healing will result in the formation of calcium (bone) within the plantar fascia. When this occurs adjacent to the heel bone it is known as heel spurs, which have a longer rehabilitation period.
Diagnosis
The health care provider will perform a physical exam. This may show tenderness on the bottom of your foot, flat feet or high arches, mild foot swelling or redness, stiffness or tightness of the arch in the bottom of your foot. X-rays may be taken to rule out other problems.
Non Surgical Treatment
As with most soft tissue injuries the initial treatment is Rest, Ice, and Protection. In the early phase you’ll most likely be unable to walk pain-free. Our first aim is to provide you with some active rest from pain-provoking foot postures. This means that you should stop doing any movement or activity that provoked your foot pain in the first place. Ice is a simple and effective modality to reduce your pain and swelling. Please apply for 20-30 minutes each 2 to 4 hours during the initial phase or when you notice that your injury is warm or hot. A frozen water bottle can provide you with a ice foot roller that can simultaneously provide you with some gentle plantar fascia massage. Anti-inflammatory medication (if tolerated) and natural substances eg arnica may help reduce your pain and swelling. However, it is best to avoid anti-inflammatory drugs during the initial 48 to 72 hours when they may encourage additional bleeding. Most people can tolerate paracetamol as a pain reducing medication. To support and protect your plantar fascia, you may need to be wear a plantar fascia brace, heel cups or have your foot taped to provide pain relief. As mentioned earlier, the cause of your plantar fasciitis will determine what works best for you. Your physiotherapist will guide you. Your physiotherapist will guide you and utilise a range of pain relieving techniques including joint mobilisations for stiff joints, massage, electrotherapy, acupuncture or dry needling to assist you during this pain-full phase.

Surgical Treatment
Surgery is usually not needed for plantar fasciitis. About 95 out of 100 people who have plantar fasciitis are able to relieve heel pain without surgery. Your doctor may consider surgery if non-surgical treatment has not helped and heel pain is restricting your daily activities. Some doctors feel that you should try non-surgical treatment for at least 6 months before you consider surgery. The main types of surgery for plantar fasciitis are Plantar fascia release. This procedure involves cutting part of the plantar fascia ligament . This releases the tension on the ligament and relieves inflammation . Other procedures, such as removing a heel spur or stretching or loosening specific foot nerves. These surgeries are usually done in combination with plantar fascia release when there is lasting heel pain and another heel problem. Experts in the past thought that heel spurs caused plantar fasciitis. Now experts generally believe that heel spurs are the result, not the cause, of plantar fasciitis. Many people with large heel spurs never have heel pain or plantar fasciitis. So surgery to remove heel spurs is rarely done.
Stretching Exercises
You may begin exercising the muscles of your foot right away by gently stretching them as follows. Prone hip extension, Lie on your stomach with your legs straight out behind you. Tighten up your buttocks muscles and lift one leg off the floor about 8 inches. Keep your knee straight. Hold for 5 seconds. Then lower your leg and relax. Do 3 sets of 10. Towel stretch, Sit on a hard surface with one leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your knee straight. Hold this position for 15 to 30 seconds then relax. Repeat 3 times. When the towel stretch becomes too easy, you may begin doing the standing calf stretch. Standing calf stretch, Facing a wall, put your hands against the wall at about eye level. Keep one leg back with the heel on the floor, and the other leg forward. Turn your back foot slightly inward (as if you were pigeon-toed) as you slowly lean into the wall until you feel a stretch in the back of your calf. Hold for 15 to 30 seconds. Repeat 3 times. Do this exercise several times each day. Sitting plantar fascia stretch, Sit in a chair and cross one foot over your other knee. Grab the base of your toes and pull them back toward your leg until you feel a comfortable stretch. Hold 15 seconds and repeat 3 times. When you can stand comfortably on your injured foot, you can begin standing to stretch the bottom of your foot using the plantar fascia stretch. Achilles stretch, Stand with the ball of one foot on a stair. Reach for the bottom step with your heel until you feel a stretch in the arch of your foot. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. After you have stretched the bottom muscles of your foot, you can begin strengthening the top muscles of your foot. Frozen can roll, Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if done first thing in the morning. Towel pickup, With your heel on the ground, pick up a towel with your toes. Release. Repeat 10 to 20 times. When this gets easy, add more resistance by placing a book or small weight on the towel. Balance and reach exercises, Stand upright next to a chair. This will provide you with balance if needed. Stand on the foot farthest from the chair. Try to raise the arch of your foot while keeping your toes on the floor. Keep your foot in this position and reach forward in front of you with your hand farthest away from the chair, allowing your knee to bend. Repeat this 10 times while maintaining the arch height. This exercise can be made more difficult by reaching farther in front of you. Do 2 sets. Stand in the same position as above. While maintaining your arch height, reach the hand farthest away from the chair across your body toward the chair. The farther you reach, the more challenging the exercise. Do 2 sets of 10. Heel raise, Balance yourself while standing behind a chair or counter. Using the chair to help you, raise your body up onto your toes and hold for 5 seconds. Then slowly lower yourself down without holding onto the chair. Hold onto the chair or counter if you need to. When this exercise becomes less painful, try lowering on one leg only. Repeat 10 times. Do 3 sets of 10. Side-lying leg lift, Lying on your side, tighten the front thigh muscles on your top leg and lift that leg 8 to 10 inches away from the other leg. Keep the leg straight. Do 3 sets of 10.
What Is Pain Of The Heel

Overview
The Plantar Fascia is a broad, thick band of tissue that runs from under the heel to the front of the foot. Through overuse the fascia can become inflamed and painful at its attachment to the heel bone or calcaneus. The condition is traditionally thought to be inflammation, however this is now believed to be incorrect due to the absence of inflammatory cells within the fascia. The cause of pain is thought to be degeneration of the collagen fibres close to the attachment to the heel bone.
Causes
Plantar fasciitis is the most common injury of the plantar fascia and is the most common cause of heel pain. Approximately 10% of people have plantar fasciitis at some point during their lifetime. It is commonly associated with long periods of standing and is much more prevalent in individuals with excessive inward rolling of the foot, which is seen with flat feet. Among non-athletic populations, plantar fasciitis is associated with obesity and lack of physical exercise.
Symptoms
The classic sign of plantar fasciitis is that the worst pain occurs with the first few steps in the morning, but not every patient will have this symptom. Patients often notice pain at the beginning of activity that lessens or resolves as they warm up. The pain may also occur with prolonged standing and is sometimes accompanied by stiffness. In more severe cases, the pain will also worsen toward the end of the day.
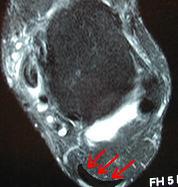
Diagnosis
During the physical exam, your doctor checks for points of tenderness in your foot. The location of your pain can help determine its cause. Usually no tests are necessary. The diagnosis is made based on the history and physical examination. Occasionally your doctor may suggest an X-ray or magnetic resonance imaging (MRI) to make sure your pain isn't being caused by another problem, such as a stress fracture or a pinched nerve. Sometimes an X-ray shows a spur of bone projecting forward from the heel bone. In the past, these bone spurs were often blamed for heel pain and removed surgically. But many people who have bone spurs on their heels have no heel pain.
Non Surgical Treatment
First check your shoes for too much midfoot flexibility and check your training for changes. A detailed evaluation of changes in your training is necessary. You should start with what is called "relative rest" which means a decrease in workout intensity, duration of session and decrease in the number of sessions per week. The most important part of self treatment for this condition is being sure that your shoes offer sufficient stability and are optimal in controlling the forces that contribute to plantar fasciitis and heel spurs. Check your running shoes to make sure that they are not excessively worn. They should bend only at the ball of the foot, where your toes attach to the foot. This is vital! Avoid any shoe that bends in the center of the arch or behind the ball of the foot. It offers insufficient support and will stress your plantar fascia. The human foot was not designed to bend here and neither should a shoe be designed to do this. You should also be doing gentle calf stretching exercises. This will reduce stress on the plantar fascia in two ways. The first manner in which a relaxation of the tension in the calf muscles can help heel pain is that it will reduce the direct pull backwards on the heel bone (calcaneus). The second reason is a little bit more complicated, but essentially it is that a tight achilles tendon and calf muscles causes the rearfoot to move in a manner that causes over pronation as your leg and body move forward over your foot. So go ahead and gently stretch the calf muscle by doing the runner's wall leaning stretch. To strengthen the muscles in your arch toe curls or "doming" can be done. Toe curls may be done by placing a towel on a kitchen floor and then curling your toes to pull the towel towards you. This exercise may also be done without the towel against the resistance of the floor.
Surgical Treatment
In cases that do not respond to any conservative treatment, surgical release of the plantar fascia may be considered. Plantar fasciotomy may be performed using open, endoscopic or radiofrequency lesioning techniques. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. Potential risk factors include flattening of the longitudinal arch and heel hypoesthesia as well as the potential complications associated with rupture of the plantar fascia and complications related to anesthesia.
Prevention
Plantar fasciitis can be a nagging problem, which gets worse and more difficult to treat the longer it's present. To prevent plantar fasciitis, run on soft surfaces, keep mileage increases to less than 10 percent per week, and visit a specialty running shop to make sure you're wearing the proper shoes for your foot type and gait. It's also important to stretch the plantar fascia and Achilles tendon.
What Is Painful Heel And Tips To Prevent It

Overview
Plantar fasciitis is a condition that causes heel and arch pain through inflammation on the bottom of the foot. The part that’s inflamed (swollen) is actually the plantar fascia, which is the connective tissue or ligament that stretches from the base of the toes, across the arch of the foot, and inserts into the heel bone. This painful condition can interfere with your daily activity and severely decrease your quality of life.
Causes
Plantar fasciitis most commonly occurs due to repetitive or prolonged activities placing strain on the plantar fascia. It is often seen in runners, or dancers and gymnasts who perform regular activities involving end of range foot and ankle movements. It may also occur in patients who walk excessively, especially up hills or on uneven surfaces. Older patients who spend a lot of time on their feet may also develop the condition. Plantar fasciitis frequently occurs in association with calf muscle tightness, inappropriate footwear, or biomechanical abnormalities, such as excessive pronation (flat feet) or supination (high arches). Occasionally the condition may occur suddenly due to a high force going through the plantar fascia beyond what it can withstand. This may be due to activities such as a sudden acceleration or a forceful jump.
Symptoms
Symptoms of plantar fasciitis include pain in the heel of the foot. Some people complain of a sharp stabbing pain especially with walking. Others describe the pain as a dull ache after prolonged standing. The pain of plantar fasciitis is often worst in the morning or following activity.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
Most health care providers agree that initial treatment for plantar fasciitis should be quite conservative. You'll probably be advised to avoid any exercise that is making your pain worse. Your doctor may also advise one or more of these treatment options. A heel pad. In plantar fasciitis, a heel pad is sometimes used to cushion the painful heel if you spend a great deal of time on your feet on hard surfaces. Also, over-the-counter or custom-made orthotics, which fit inside your shoes, may be constructed to address specific imbalances you may have with foot placement or gait. Stretching: Stretching exercises performed three to five times a day can help elongate the heel cord. Ice: You may be advised to apply ice packs to your heel or to use an ice block to massage the plantar fascia before going to bed each night. Pain relievers: Simple over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are often helpful in decreasing inflammation and pain. If you have stomach trouble from such drugs, your health care provider may prescribe an alternative. A night splint: A night splint is sometimes used to hold your foot at a specific angle, which prevents the plantar fascia from shortening during sleep. Ultrasound: Ultrasound therapy can be performed to decrease inflammation and aid healing. Steroid injections: Anti-inflammatory steroid injections directly into the tissue around your heel may be temporarily helpful. However, if these injections are used too many times, you may suffer other complications, such as shrinking of the fat pad of your heel, which you need for insulation. Loss of the fat pad could actually increase your pain, or could even rupture the plantar fascia in rare cases. Walking cast: In cases of long-term plantar fasciitis unresponsive to usual treatments, your doctor may recommend that you wear a short walking cast for about three weeks. This ensures that your foot is held in a position that allows the plantar fascia to heal in a stretched, rather than shortened, position. Shock wave therapy, Extracorporeal shock wave therapy which may be prescribed prior to considering surgery if your symptoms have persisted for more than six months. This treatment does not involve any actual incisions being made rather it uses a high intensity shock wave to stimulate healing of the plantar fascia.

Surgical Treatment
Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted. The most common complications of release surgery include incomplete relief of pain and nerve damage.
Exercises For Diabetic Peripheral Neuropathy
TOE CONDITIONS: Ingrown toenails, blood accumulation under the nail plate (subungual hematoma), corns and calluses are all often seen as a result of playing baseball. It is important that good foot hygiene be practiced with washing between the toes and drying the feet well after bathing. Topical antifungals work well to treat athletes foot. ORTHOPEDIC INJURIES: Most orthopedic baseball foot and ankle injuries are acute or sudden. If an individuals foot or ankle is injured, seek immediate evaluation with one of our doctors. If your athlete has a baseball related injury, call our specialists at Advanced Foot and Ankle Center in McKinney and Prosper Texas at 972-542-2155. However, toe numbness and pain occurring together is one such problem that you cannot afford to ignore. Common symptoms are flat feet knee problems , burning sensation, numbness.
Most flat feet usually do not cause pain or other problems. Flat feet may be associated with pronation, a leaning inward of the ankle bones toward the center line. Foot pain, ankle pain or lower leg pain, especially in children, may be a result of flat feet and should be evaluated.

Do not consume food items which you are allergic to. Keep dead skin off your lips by lightly scrubbing them at least twice a week using a mild, natural ingredient such as cornflour or a lemon juice-sugar pack. I had a long road workout two weeks ago and immediately after starting having pain on the ball of my foot in this area. I have also learned buying shoes online is easy.

Bunions are bony lumps that develop on the side of your foot and at the base of your big toe. They're the result of a condition called hallux valgus, which causes your big toe joint to bend towards your other toes and become may also develop a bursa here too, especially if your shoes press against the bunion. Sometimes swellings or bursae on the joints in your feet are also called bunions, but these aren't the same as bunions caused by hallux valgus. Hallux valgus is different to hallux rigidus, which is osteoarthritis of the big toe joint. Hallux rigidus causes your big toe to become stiff and its range of movement is reduced. Symptoms of a bunion can be controlled by choosing shoes with a soft, wide upper to reduce pressure and rubbing on your joint. Toes form hammer or claw shape.
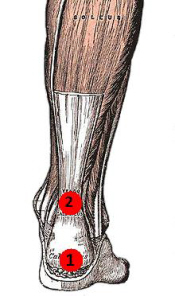
Achilles Tendinitis
 Achilles Tendonitis is a term that commonly refers to an inflammation of the Achilles tendon or its covering. It is an overuse injury that is common especially to joggers and jumpers, due to the repetitive action and so may occur in other activities that requires the same repetitive action. Most experts now use the term Achilles tendinopathy to include both inflammation and micro-tears. But many doctors may still use the term tendonitis out of habit.
Achilles Tendonitis is a term that commonly refers to an inflammation of the Achilles tendon or its covering. It is an overuse injury that is common especially to joggers and jumpers, due to the repetitive action and so may occur in other activities that requires the same repetitive action. Most experts now use the term Achilles tendinopathy to include both inflammation and micro-tears. But many doctors may still use the term tendonitis out of habit.
Causes
Achilles tendonitis is an overuse injury. Too much too soon is the common cause of overuse injuries, however other factors can contribute to developing the condition. An increase in activity, either distance, speed or a sudden change to running up hills. As a rule of thumb distance runners should increase their mileage by no more than 10% per week. A change of footwear or training surface for example suddenly running on soft sand can cause the heel to drop lower than normal making the tendon stretch further than it is used to. Weak calf muscles can tighten or go into partial spasm which again increases the strain on the achilles tendon by shortening the muscle. Running up hills - the achilles tendon has to stretch more than normal on every stride. This is fine for a while but will mean the tendon will fatigue sooner than normal. Overpronation or feet which roll in when running can place an increased strain on the achilles tendon. As the foot rolls in (flattens) the lower leg also rotates inwards which places twisting stresses on the tendon. Wearing high heels constantly shortens the tendon and calf muscles. When exercising in flat running shoes, the tendon is stretched beyond its normal range which places an abnormal strain on the tendon.
Symptoms
Most cases of Achilles tendonitis start out slowly, with very little pain, and then grow worse over time. Some of the more common symptoms include mild pain or an ache above the heel and in the lower leg, especially after running or doing other physical activities, pain that gets worse when walking uphill, climbing stairs, or taking part in intense or prolonged exercise, stiffness and tenderness in the heel, especially in the morning, that gradually goes away, swelling or hard knots of tissue in the Achilles tendon, a creaking or crackling sound when moving the ankle or pressing on the Achilles tendon, weakness in the affected leg.
Diagnosis
To confirm the diagnosis and consider what might be causing the problem, it?s important to see your doctor or a physiotherapist. Methods used to make a diagnosis may include, medical history, including your exercise habits and footwear, physical examination, especially examining for thickness and tenderness of the Achilles tendon, tests that may include an x-ray of the foot, ultrasound and occasionally blood tests (to test for an inflammatory condition), and an MRI scan of the tendon.
Nonsurgical Treatment
The aim of the treatment is to reduce strain on the tendon and reduce inflammation. Strain may be reduced by, avoiding or severely limiting activities that may aggravate the condition, such as running, using shoe inserts (orthoses) to take pressure off the tendon as it heals. In cases of flat or hyperpronated feet, your doctor or podiatrist may recommend long-term use of orthoses. I8nflammation may be reduced by, applying icepacks for 20 minutes per hour during the acute stage, taking non-steroidal anti-inflammatory drugs, placing the foot in a cast or restrictive ankle-boot to minimise movement and give the tendon time to heal. This may be recommended in severe cases and used for about eight weeks. Occasionally depot (slowly absorbed) steroid injections may be tried, particularly for peri-tendinitis, but great care needs to be taken to avoid injecting into the tendon. This should only be done by a specialist doctor. You may also be given specific exercises to gently stretch the calf muscles once the acute stage of inflammation has settled down. Your doctor or physiotherapist will recommend these exercises when you are on the road to recovery. Recovery is often slow and will depend on the severity of the condition and how carefully you follow the treatment and care instructions you are given.
Surgical Treatment
Treating this surgically, there are numerous methods to repair the tendon. Most commonly, Achilles tendon is exposed through an incision at the back of the ankle. After identifying both ends of ruptured tendon, the edges got trimmed and then both ends were sutured together with optimal tension. To get a better outcome with fixation, an anchor may have to be in place in calcaneus, provided the rupture is very low. Care must be taken to avoid injuries to the nerves located adjacent to the tendon.
Prevention
Your podiatrist will work with you to decrease your chances of re-developing tendinitis. He or she may create custom orthotics to help control the motion of your feet. He or she may also recommend certain stretches or exercises to increase the tendon's elasticity and strengthen the muscles attached to the tendon. Gradually increasing your activity level with an appropriate training schedule-building up to a 5K run, for instance, instead of simply tackling the whole course the first day-can also help prevent tendinitis.
What Every Vibrant Woman Should Know
Most foot and ankle surgeries are day surgeries, which means you will go home the day of surgery. Keep your foot elevated as much as possible for the first week after your foot dry for at least 2 weeks after week after surgery you will have your dressing changed by coming to see your attending sutures will be removed after the second doctor will advise you when you can increase activities and put weight on the pain and anti-inflammatory medications as prescribed by your physician.Vitamin C is important to heal scar tissue. Take 4,000 mg spread out over each day in 500 mg doses taken for several days to several weeks after surgery.Omega 3 fatty acids, such as flax or fish oil, vitamin A and beta-carotene aid in the skin healing and lessen the appearance of scars.
Please�make an appointment with Dr. Morris or Dr. Boggs at the�Everett Podiatric Sports Medicine clinic today! If the pain is resolved, then you can assume that your shoes were the cause. But, a quick look at them will show that they are, for the most part, poorly designed for good foot health. It's okay to wear high heels or dress shoes with pointy toes, as long as you only do so occasionally. A variety of toe deformities occur in children's feet.
Foot care is an essential routine activity that should be done by all individuals to achieve optimum wellness. Foot is a significant part of your physique therefore, you should value it. You must be mindful that there are lots of approaches to protect yourself from foot ailments. Reflexology is an ancient art of applying pressure and massage to reflex points on the foot. Reflexology treatment is aimed to give complete relaxation and overall benefits through foot reflex manipulation and general foot and lower leg massage. Hammer toe is more likely to simultaneously occur with bunions.

Any of your several types of nerves can be affected: your sensory nerves (which provide information about sensation, such as pain or heat), motor nerves (which carry signals to your muscles to provide tone and movement), or your autonomic nerves (which control reflexive, or non-voluntary body functions, such as breathing, heartbeats, and digestion). Well, kind of. Losing motor nerves in the foot may mean that the muscles in your feet will weaken. This weakening can cause deformities such as claw toe (toes that curl down into the soles of your shoes like bird claws), which can lead to serious discomfort as they rub against the inside of your shoe and form calluses. If coupled with sensory nerve damage, these calluses can become serious problems. Imagine you have an infected toenail. Now, imagine if you still had that infected toenail, but couldn't feel it. Or if you had a blister on the bottom of your foot and kept walking on it. Or a splinter. They look similar to Oribis.

The cartilage begins to deteriorate and that in turn causes the bones to rub together which is what results in pain, stiffness, loss of mobility and finally disability. In order to get to the root of the problem and not simply manage pain, here are a few suggestions and natural supplements that have been shown to improve the condition as well as relieve pain without the dangers of NSAID drugs. One of the primary treatments you should consider including is a good source of animal-based Omega-3 fats like krill or cod liver oil. One of the most promising natural substances is a plant enzyme found in pineapple called bromelain.
The surgeon may also remove a small section of bone, and repair tendons and ligaments if necessary. In this procedure, the surgeon inserts a silicone rubber or metal implant specially designed for the toe to replace the gliding surfaces of the joint and act as a joint spacer. Patients usually consult a doctor about toe deformities because of pain or discomfort in the foot when walking or running. The physician takes several factors into consideration when examining a patient who may require surgery to correct a toe deformity. American College of Foot and Ankle Surgeons.
Hammertoe And Mallet Toe
Conventional Putter - Use this golf club putter, if you could, in other words, at least start with a conventional putter. That's what pro's are teaching us. So let us be well-behaved! Concentrate on you putting line and go! Heel Toe Weighted - The weight has been distributed equally to the heel and toe - sometimes by using inserts (see under Insert), sometimes by a cavity designed center. Meant to make, according to manufacturers, the lady golf putter more forgiving. Perimeter Weighted - The weight has been distributed over the edges of the head, creating a largers sweetspot, therefore these lady golf putters forgive more mishits. Everyday when we are out doing a demo day for our Ashdon Putters, I am rewarded and encouraged by a customers satisfaction and comments. Recently, while working at a Country Club in the San Diego area, Mr. Fritz Long stated that this is the best putter I have ever had. Once the ball is hit it stays on line and has a true roll. I couldnt explain the results of our putters any better than his statement. Broomstick Golf Club Putter or Long Putter - Longer than all other lady golf putters. This lady golf club is difficult. You have to be sure about your technique to control this one. Wedges are genuinely just specialty irons. the initial wedge will be Pitching Wedge (PW), that is commonly involving 52 and 56 degrees in loft. The PW will be greatest lofted metal inside a common specified and most affordable loft of your wedges. Lob wedges variety from 58 to 64 degrees and so are utilized for near variety brief and higher shots to prevail over obstacles near towards green. Ping G15 Driver Wedges are really beneficial for the brief video game and it's always effective to preserve a choice of them as section of your bag. I'd brought an exfoliating foot cream which I used over the entire foot. The soles of his feet were smooth when I was finished but the callous was incredibly tough. I had brought a pumice stone and tried to use it on his big toe but the sensation was not pleasant for him. In a small bottle, I had a combination of essential oils prepared for the relief of pain. I slowly massaged the oil into his foot. I finished by painting a couple drops of salicylic acid liquid across the callous and bandaging his toe with gauze and tape. Then I slipped a clean sock onto his foot. In addition, This Titleist California Sonoma Putter also allows you to change the lie angle by up to +/- 2 degrees from the standard 71 degree lie angle and features a drafted sole to keep the putter head square for proper alignment, along with a high toe setup to reduce the temptation of raising the toe end up at address, which leads to aiming left of target. If you are using the wrong golfing equipment,such as golf drivers and putters, you will quickly find that you willnot play as well as someone who has the right equipment. With this deformity, the toe is bent at the middle joint causing a curling of the toe. It is most common in the second toe, but can occur in any toe. Hammer toes are often present along with a bunion, a painful outgrowth along the side of the foot at the base of the big toe. This deformity is very similar to a hammer toe except the joint involved is the upper joint instead of the middle joint, giving the toe a mallet-like appearance at the end of the toe. Spinal cord or peripheral nerve damage may cause all of your toes to curl downward. Risk Factors for a Hammertoe For diagonal stair supports, use 2x12" boards (or logs), to fit the space. Cut the ends to fit flush with the header, and try to notch it where it meets the footer. (You can use a footer across pier blocks, too, as long as it's tied to the other supports. Use a horizontal tie to connect the bottom footer with the top support, if there is any chance that the bottom support can give or slide outward.). These directions are intended for a simple deck or front stoop. Ask your local building supply (or builders you may know) for any tips on building in your particular location or situation.
I'd brought an exfoliating foot cream which I used over the entire foot. The soles of his feet were smooth when I was finished but the callous was incredibly tough. I had brought a pumice stone and tried to use it on his big toe but the sensation was not pleasant for him. In a small bottle, I had a combination of essential oils prepared for the relief of pain. I slowly massaged the oil into his foot. I finished by painting a couple drops of salicylic acid liquid across the callous and bandaging his toe with gauze and tape. Then I slipped a clean sock onto his foot. In addition, This Titleist California Sonoma Putter also allows you to change the lie angle by up to +/- 2 degrees from the standard 71 degree lie angle and features a drafted sole to keep the putter head square for proper alignment, along with a high toe setup to reduce the temptation of raising the toe end up at address, which leads to aiming left of target. If you are using the wrong golfing equipment,such as golf drivers and putters, you will quickly find that you willnot play as well as someone who has the right equipment. With this deformity, the toe is bent at the middle joint causing a curling of the toe. It is most common in the second toe, but can occur in any toe. Hammer toes are often present along with a bunion, a painful outgrowth along the side of the foot at the base of the big toe. This deformity is very similar to a hammer toe except the joint involved is the upper joint instead of the middle joint, giving the toe a mallet-like appearance at the end of the toe. Spinal cord or peripheral nerve damage may cause all of your toes to curl downward. Risk Factors for a Hammertoe For diagonal stair supports, use 2x12" boards (or logs), to fit the space. Cut the ends to fit flush with the header, and try to notch it where it meets the footer. (You can use a footer across pier blocks, too, as long as it's tied to the other supports. Use a horizontal tie to connect the bottom footer with the top support, if there is any chance that the bottom support can give or slide outward.). These directions are intended for a simple deck or front stoop. Ask your local building supply (or builders you may know) for any tips on building in your particular location or situation.